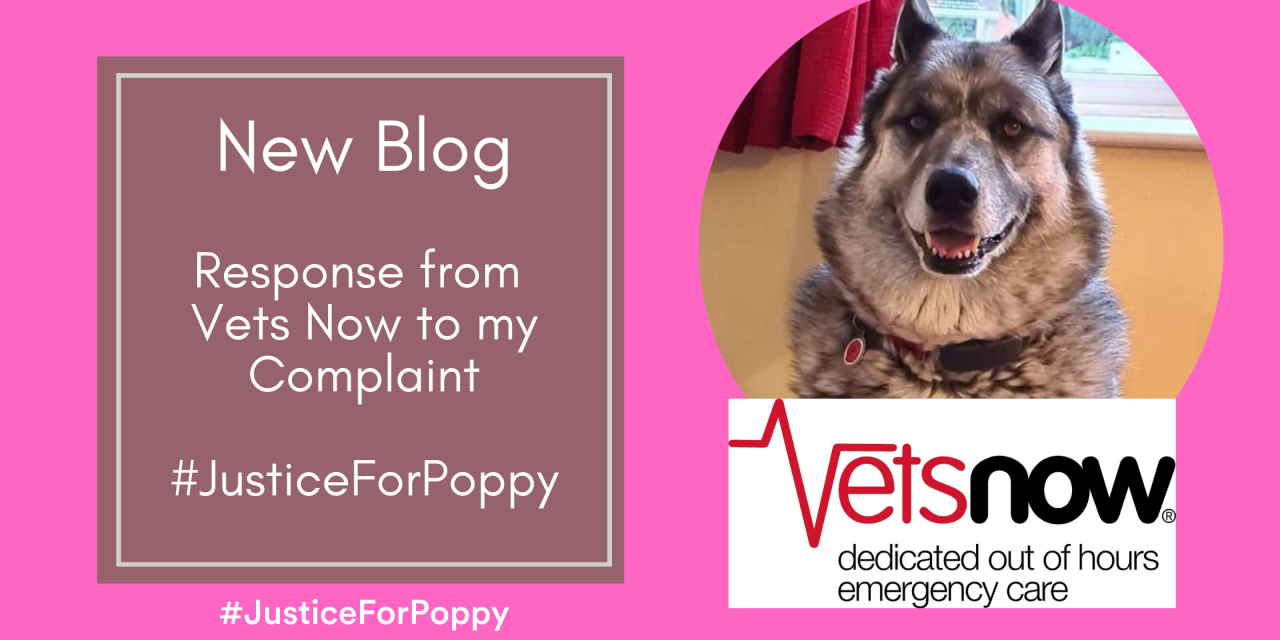
I have now had a response from Vets Now in relation to the complaint I put in about the treatment my beloved dog Poppy received at Vets Now Worcester in early July. I have removed all identifiable information but left the email address in for their complaints department in case anyone reading this needs to put in a complaint to Vets Now. I’m very pleased that they have taken my complaint seriously and will learn from what happened to hopefully avoid someone else going through what we went through with Poppy. The response is copied below:
Thank you for your communication on 7 July outlining concerns following your visit to our Vets Now Worcester clinic with Poppy on 5 July and I apologise for the delay in responding to you. I am sorry to learn that you were dissatisfied with the level of service you received during your visit. We aim to provide the highest levels of patient and customer care and strive to continually improve our service. I am sorry that we were unable to reflect this during your recent experience, and you feel that Vets Now have let you down on this occasion.
It is my understanding you have some concerns, specifically:
- you believe that Poppy experienced a very severe adverse reaction to the opioid pain relief provided at our clinic.
- you report that Poppy needed your care and attention throughout the night with her severe discomfort.
- you feel that if you had known the risks and side effects beforehand, you would not have consented to her receiving this medication for the benefit of sleep.
- you were shocked to be advised to “just ride it out” when you contacted the clinic for advice at 3:30am.
- on attending Stocks Vets, you understood from speaking to your vet that Poppy had experienced significant side effects from the buprenorphine given. You understood that their recommendation to admit her to their practice for further medical care was a consequence of this.
- you feel that the distress and inconvenience of Poppy’s condition was completely avoidable, and you were not able to make an informed decision about her care.
I also understand that your preferred outcome of this complaint is specifically detailed in the following outcomes:
-
- An apology
- Investigation of why you were not given the information you needed to make a decision
- Review of the information provided when consulting patients’ families
- Revision of your invoice, removing the charge for buprenorphine
- Compensation for many hours of distress, worry and inconvenience
- Cover the costs of the subsequent treatment Poppy had at The Stocks Veterinary Centre
I have taken time to review your correspondence, read the clinical notes and liaise with the staff on duty to help with my investigation into your concerns and I am now in a position to respond.
I am very sorry to hear of the upsetting events precipitating your submission of a complaint. I wish to assure you that I have taken your concerns seriously in addressing Poppy’s case. I understand that following Poppy’s return home from our clinic, she displayed signs of abnormal behaviour which you understandably found very concerning. I appreciate that your highest priority is Poppy’s comfort and wellbeing, and you felt that this was not preserved by the treatment she received.
I appreciate that you have performed your own research into the use and potential side effects of buprenorphine, at the following links:
I note that their extended list of side effects comprises excessive drowsiness, slow breathing rate, nausea, vomiting, low heart rate, agitation (panting, purring, pacing, whining, hiding), loss of appetite, drooling, dilated pupils and constipation.
This is a question-and-answer forum with responses from an anonymous respondent who has been certified by the website as a vet, who self-reports to be based in the USA. They advise that anxiety in older dogs is common, and this can be increased in patients when opioid medication is wearing off. I do not intend to discredit the advice provided but the relevance and specificity of advice given anonymously online must always be considered.
On review of the publicly accessible datasheet for the exact medication used (available at: https://www.noahcompendium.co.uk/?id=-448842), the listed side-effects you describe (restlessness, excessive panting, excessive whining and excessive movement) are not described as severe. Patients exhibiting significant changes in their cardiorespiratory function (abnormally slow heart rate, abnormally slow breathing rate, significantly depressed demeanour or collapse) would be considered to be exhibiting severe side effects warranting emergency management or use of opioid reversal agents to stabilise their condition.
Thank you for providing the CCTV footage from the camera in your kitchen to demonstrate Poppy’s behaviour. Online access via YouTube was an innovative solution to the challenges of sharing media and I will look to utilise this when reviewing video in future, as it is far easier to understand the context of your concerns. In the first video (Poppy Footage 1 6 July 2024), Poppy stands on the mats on the right side of frame, whines and pants lightly. She initially seems unwilling to step off the small mat she is standing on, although multiple other mats are in reach. Forty-two seconds into the recording, she steps off the mat and walks out of the bottom of the frame, and does not reappear for twenty-six seconds, when you enter the view of the camera and follow her to the door. She then stands in the doorway with you, until you close the door. In the second video (Poppy Footage 2 6 July 2024), she walked with a calm, coordinated gait from the door at the top right of the frame to a location out of frame and remained out of view for approximately 55 seconds, then re-entered view and returned to the door, stood by it, and whined. You followed her around the room, and when you opened the door, she walked out in a calm, coordinated gait. From these videos, I can see that Poppy was not settled and sleeping as you or I would expect a dog to be in the early hours of the morning, excluding any pre-existing habits of moving around the house at night, and I appreciate how concerning this would be for you and why you would wish to provide her with your care and attention throughout the night.
Opioid analgesic use is considered and recommended on an individual basis. Opioid medications are widely understood to be excellent analgesics, but their method of action in the body means they are not suitable for every patient, particularly those with cardiac or respiratory disease, and use in those circumstances must be carefully consider. Likewise, some patients who are otherwise outwardly well may be more sensitive to a normal dose than anticipated.
I am sorry that Poppy was unsettled overnight following provision of supportive medical treatment. It is my understanding that your initial concern when presenting her to our Worcester clinic was that she was displaying signs of discomfort, pacing, unable to settle, and would not lie down. I regret that I cannot determine a significant difference between this description of your concerns about her discomfort at the time of attending our clinic, and the video of Poppy’s condition afterward overnight. I note that there is no significant improvement, but likewise there is no clear worsening.
I understand from your communication to us that Philippa advised you at the time that it would make Poppy sleepy or drowsy, which you felt would be good and help her to settle and sleep. Philippa has reflected that though some dogs can pant when given buprenorphine, it is a medication which is widely used without complications, and she did not feel it was relevant to discuss every possible adverse event of each drug at the time. I likewise would not provide a full list of every potential side-effect of every medication recommended or given to a patient, as this is unrealistic and broadly unnecessary, unless there are particular concerns about the risk of an adverse event due to an individual patient’s condition or wider circumstances. I would consider it entirely reasonable to advise a client that the level of opioid pain relief provided by buprenorphine should reduce pain, likely help with relaxation and could make a patient more sleepy or wobbly, as I recognise that this could be a source of concern and recommend that any worries about the patient’s condition should be reported to a vet for advice. I am sorry that this was not a satisfactory level of information for you to feel that informed consent could be provided. I hope that you felt you had sufficient opportunity to ask any questions about Poppy’s care at the time of your consultation.
All vets make their decisions and recommendations based upon the findings of their examination and their understanding of the wider circumstances of the case at the time. From an external and retrospective viewpoint, your options at that time would be:
- The supportive medication plan (anti-sickness medication and buprenorphine) recommended by Philippa.
- Adjustment of the analgesic options, with either:
- Placement of an intravenous catheter in order to administer intravenous paracetamol medication, which involves additional handling, and some patients can find this particularly stressful.
- Prescribing paracetamol-based medication to be given orally and continued by you at home. As I understand that Poppy would not eat or take oral medications, I do not feel that this was likely to be successful in significantly improving her comfort.
- NB. Other pain relief options, such as non-steroidal anti-inflammatory medications (Metacam, Loxicom) are not appropriate for patients with gastrointestinal disease and can worsen vomiting or diarrhoea.
- Declining to provide medication, as despite her reported behaviour at home, her clinical examination yielded no abnormal findings.
With this in mind, the intention of providing the recommended treatment was to improve Poppy’s perceived discomfort and provide you with peace of mind. The alternatives were likely to be less successful or not provide any benefit at all.
I am aware that you contacted the clinic in the early hours of the morning of 6th July. I regret that I am unable to find any record of telephone conversations received by our clinic at 3:30am, but I have been able to review that recorded conversation had at around 1:30am. I understand from Shannon, the nurse who was working at the clinic that night and triaged Poppy for you on arrival, that she discussed Poppy with the vet when you called at 1:30am. During this call, she confirmed to you that administration of the pain relief may have made Poppy confused, but that her pain should be controlled. She passed on advice from the vet to administer paracetamol if you had this at home. When you expressed concerns that Poppy’s signs were more severe, she advised that the alternative was for Poppy to be admitted to the clinic for supportive care and monitoring, and that opioid pain relief could not be repeated as it was not yet due. You expressed that you did not feel Poppy was in pain but was uncomfortable or possibly reacting to what she had been given, and you reported that she had never had an issue before. Shannon spoke to vet again for you. She reiterated that further pain relief could not be given, as that had not yet worn off. Shannon advised you that if you wanted further investigations, you would have to be redirected to an alternative clinic, as the vet would be working alone from 3am and it would not be appropriate to sedate Poppy in that situation. You were advised to contact the Birmingham clinic if you wished to pursue this, as the team there would be able to facilitate investigation of your concerns. In summarising the call, Shannon confirmed to you again that no other medication could be provided to change Poppy’s condition at that time, and she confirmed to you when you asked that the effects of buprenorphine would last for up to eight hours. At the very end of this call, Shannon advised that other than presenting Poppy for reassessment or providing additional pain relief at home, the only alternative option was to “ride it out”. On receipt of your complaint, I was concerned at the implications of this phrase as you described it. In the context of the recorded conversation, I understand that Shannon communicated twice with the vet in the clinic on your behalf and explained all of the options available to you. I am dismayed by the phrasing used and appreciate how this would have been upsetting for you, but I do not feel that there was any ill-intent in this advice, nor do I get the impression that your concerns were being dismissed or Poppy’s condition ignored. You were provided with options for further management and intervention, or to continue monitoring her progress at home.
In the absence of any reports of contact with our Birmingham clinic, I must assume that you did opt to monitor Poppy’s condition through the night at home. I understand that upon reassessment at Stocks Vets on the morning of 6th July, you reported that Poppy’s condition was worse and reported that Poppy had been “[panting, pacing, whining, wobbly on legs, couldn’t settle, won’t eat or drink”. Poppy was quiet and was subjectively considered “spaced out”, but her clinical examination was otherwise normal. Your vets felt that there was no progression of Poppy’s clinical disease but appropriately advised that the behavioural signs you reported had been present overnight could be secondary to opioid pain relief administration. I must again note that the same unsettled behaviours were reportedly present prior to administration of opioid pain relief, and at that time were attributed to the discomfort of her gastrointestinal issue.
Your vet at Stocks Vets discussed options for Poppy’s treatment with you, and because you had not been able to administer any medications at home, they offered to admit Poppy for intravenous fluid support and give her medications as planned, to help her feel better before the weekend. The duration of action of buprenorphine is widely accepted to be six to eight hours, and therefore I feel it is unlikely that intravenous fluids were intended to actively reduce the effect of or “flush out” residual opioid in her body, and instead would help maintain her hydration as I understand you were concerned that she had not eaten or drunk anything since around 5pm the previous evening. Poppy was given her oral medications the clinical team, ate some wet food, and was discharged at lunchtime after being given another injection of anti-sickness medication.
The treatment provided by Stocks Vets was broadly supportive and non-specific to adverse effects of opioids. As mentioned above, in the absence of severe clinical signs, there was no need to intervene significantly overnight or in the morning, nor seek opioid reversal agents to manage her condition.
At Vets Now we strive to continually improve our service, and we recognise that we can learn through the reflection of cases that have progressed unexpectedly and from receiving feedback of customers’ experiences.
Thank you again for taking the time to contact us and bring your concerns to our attention and providing us with an opportunity to discuss the events and rectify them, I trust that my explanation has given you a greater understanding of Poppy’s situation and provided the answers you need. However, please contact our team if you have questions that you would like to discuss at complaints@vets-now.com.
I hope that if I have cause to take Poppy to Vets Now in Worcester again they have learnt from my complaint and concerns, and I have also learnt that Poppy is never to have any opiod based painkiller ever again. I’m very happy that she is doing well after her ordeal, long may that continue.
#JusticeForPoppy
#VetsNow
#GreedOverNeed